How honesty may be the best policy for medical errors

Jack Gentry speaking at a 2018 Patient Safety Movement Foundation conference in Huntington Beach, California. Photo courtesy of Jack Gentry.
(NewsNation) — Thousands of medical errors occur every year in the U.S. and medical institutions have historically responded by limiting communication with the patient out of the belief it will defend them legally. But others are taking a different approach: acknowledging the mistake and taking steps to rectify it in the hospital rather than in a courtroom.
Retired Baltimore City police officer Jack Gentry is advocating for that model across the country, working for the same hospital where years earlier his life changed because of a medical error.
“You’d be surprised how many patients I talked to who said, ‘All I wanted was an apology,” he said. “I didn’t want the money. I didn’t care about the money. I want them to admit that they did something and make sure it doesn’t happen again.”
One year after he retired from the force, Gentry was plagued by two bulging discs in his neck. While undergoing surgery at MedStar Union Memorial Hospital in Baltimore, an instrument damaged his spinal cord during the procedure. He was paralyzed from the neck down for the rest of his life.
Contrary to typical industry practices, the surgeon acknowledged what had happened to the Gentry and his wife, taking full responsibility. Importantly, hospital leadership supported the surgeon’s open communication.
“That is not the norm, even 10 years later,” Gentry said. “In countless sessions that I’ve held around the country I’ve found out that this is unusual in health care. Systems don’t stand behind their doctors and doctors, therefore, aren’t open and honest with their patients.”
It turned out that the medical error in Gentry’s case was caused by a malfunctioning instrument rather than a mistake by the doctor. He spoke to his brother, who happened to be a malpractice attorney. He learned that a lawsuit could take many years to resolve.
Gentry began to worry about the cost of all the medical care he’d need in the near future. MedStar reached out to him to address that concern.
“They actually came to me while I was still in the hospital and said, ‘Don’t worry about any of that. We’re going to cover everything,” he said.
MedStar also settled with him on financial compensation two years after the incident (one study found that on average it takes five years for a medical malpractice suit to go through the system).
A new way to respond to MEDICAL ERRORS
William Newman, a psychiatry professor at Saint Louis University School of Medicine who has studied medical malpractice issues, said physicians are often taught to stay quiet if something goes wrong.
“Your risk management team will often say, ‘We don’t want the perception that we did something wrong encouraging them to follow into a lawsuit,'” Newman said.
This has created a divide between physicians and patients that often leads to an adversarial relationship following a medical error.
In response, the approach called Communication and Optimal Resolution (CANDOR) was created to improve communication and resolution processes. Under the approach, providers clearly communicate to patients affected by medical errors what happened and how they can work towards a resolution.
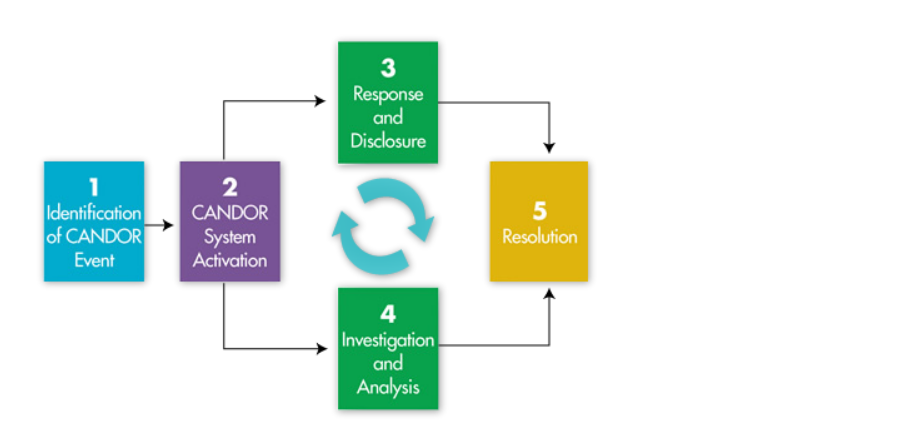
Today, CANDOR is promoted to healthcare institutions by the federal government’s Agency for Healthcare Research and Quality (AHRQ). The agency worked with 14 hospitals to test and implement the CANDOR system; by 2015, all MedStar hospitals were using it.
Along with better patient-provider relationships, the model was attractive because it ended up saving money. MedStar saved an estimated $70 million between 2012 and 2017 by reducing costs related to patient safety events, including medical liability payments.
Dave Mayer joined MedStar in 2012 as the Vice President of Quality and Safety. At that time, the system had already been experimenting with communication and resolution processes; over the next few years Mayer helped catalyze those processes and expand them.
“The programs have reduced their medical liability because the most important thing about CANDOR besides the open and honest communication is that there’s a requirement for learning,” Mayer said.
Over the 2012 to 2017 period, MedStar saw a more than 65 percent reduction in serious safety events.
The CHALLENGEs of changing medical CULTURE
While CANDOR and similar communication and resolution processes are becoming more common among healthcare institutions, many hospitals and doctors still adhere to the “deny-and-defend” model out of fear of malpractice lawsuits.
In order to encourage more open communication, many states have passed what are called “apology laws,” which make physicians’ apologies inadmissible in court in the event that a patient decides to file a malpractice lawsuit.
Newman’s research has shown that these laws have not reduced malpractice lawsuits. One reason may be that most of these laws are what are called “partial apology” laws, meaning they only protect expressions of regret, not admissions of error, which are likely less effective in building patient-doctor trust and reducing lawsuits.
He also suggested that enduring issues in medical training may be standing in the way of better practices.
“Communication is not a common part of curriculum, which is shocking,” he said. “When you’re in med school, you get very little training, historically, on how to have difficult conversations with people.”
There is some evidence, some medical schools have added instruction on apology and disclosure, according to Doug Wojcieszak, who runs the patient safety group Sorry Works!. He notes it’s a “work in progress.”
“Some schools do it well, some are just getting started,” Wojcieszak said. “Moreover, medical students are supportive of the concept and want to learn more about it, including how cases are resolved following ‘sorry.'”
Mayer emphasized that shifting a medical environment to embrace the practices of CANDOR or a similar system is a team effort.
“You cannot do this as one individual at the bedside….you have to have your CEO and your board engaged. Second is, you need to have your chief risk officer engaged,” he said.
It’s a system Gentry gravitated towards. He accepted an offer from MedStar to advocate for the hospital system’s approach to patient safety issues, and he stays in touch with the surgeon who originally operated on him.
“We’ve become friends,” he said. “He’s still my doctor. I talk to him every month or two. He’ll call me, we’ll just talk about sports or this or that, his kids or my kids.”
This story is part of NewsNation’s investigation into the tangled web of state medical malpractice laws that can make it difficult for patients and family members to file lawsuits against doctors they believe were medically negligent. Find all of our coverage on the topic here.














