SACRAMENTO, Calif. (NewsNation Now) — California has recorded a half-million coronavirus cases in the last two weeks, overwhelming emergency rooms in urban centers and rural areas including along the Mexican border where a small hospital system warns it is fast running out of patient beds.
The state could be facing a once-unthinkable caseload of nearly 100,000 hospitalizations within a month, Gov. Gavin Newsom said Monday.
Dr. Mark Ghaly, California’s secretary of Health and Human Services, said it’s feared entire areas of the state may run out of room even in their makeshift “surge” capacity units “by the end of the month and early in January.” In response, the state is updating its planning guide for how hospitals would ration care if everyone can’t get the treatment they need, he said.
“Our goal is to make sure those plans are in place, but work hard to make sure no one has to put them into place anywhere in California,” Ghaly said.
It hopes to accomplish that by beefing up temporary staffing, opening makeshift hospitals in places like gymnasiums, tents and a vacant NBA arena, and by sending patients to regions of the state that might have precious remaining beds.
California is enduring by far its worst spike in cases and hospitalizations. All of Southern California and the 12-county San Joaquin Valley to the north have been out of regular ICU capacity for days according to daily briefings by the state’s department of health.
California is averaging almost 44,000 newly confirmed cases a day and has recorded 525,000 in the last two weeks, according to data complied by Johns Hopkins University.
It’s estimated 12% of those who test positive end up in the hospital according to state models. That means 63,000 hospitalizations from the last 14 days of cases. There are currently almost 18,000 people hospitalized in the state according to state data and data complied by the COVID Tracking Project.
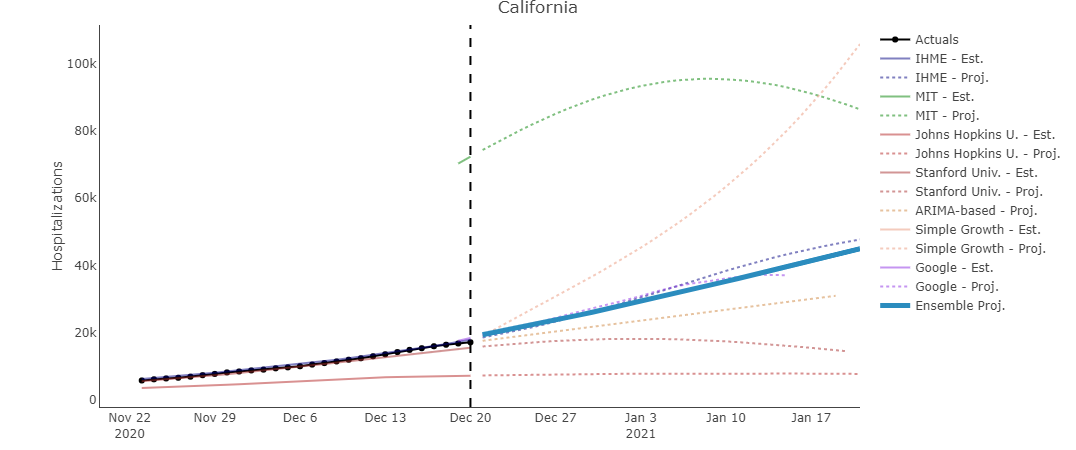
The black box (left) represents the current number of hospitalized COVID patients in California. The blue box represents the forecasted number of hospitalized patients at the 30 day mark based on models for California.
The state’s public health department in June released crisis planning guidelines for hospitals and other care facilities during the pandemic. It provides detailed guidance on how to manage care decisions when resources are scarce.
The goal is the best possible outcome for the largest number of people, the document says.
The guidelines emphasize the importance of planning for crisis scenarios and ensuring decisions are not made based on discriminatory factors such as age, race, disability, gender, socioeconomic status, insurance status.
The document outlines best practices for “proactive triage” that must occur when a hospital has exhausted its resources. A basic graphic shows the first consideration should be whether a patient is actively dying or certain to die, in which case they should only be given palliative care. You can read the full document below.
For patients not in that category, care providers are broadly asked to assess a person’s prognosis of survival compared to others when determining how to allocate limited resources.
Los Angeles is among the hardest-hit areas of the state but its hospitals aren’t there yet, LA County Department of Health Services Director Dr. Christina Ghaly said Monday. They are in the contingency stage, which means shifting around staff and equipment.
Los Angeles Mayor Eric Garcetti said experts have drawn “a straight line” between the current spikes in cases and Thanksgiving gatherings and warned people to stay home in the coming weeks.
“If you gather for the holidays, our hospitals will be overrun,” Garcetti said. “This is not a good sign, and it’s a recipe for a Christmas and New Year’s surge.”
Despite those warnings, many Californians are masked and on the move, traveling for the holiday.
“I don’t feel guilty because I do the things they say to do. I don’t just show up, without a mask, or you know, you do the common sense things. Hopefully, you’ll be protected you know,” said Brain Swanson, an air traveler.
“I’m going to see the family that I haven’t seen for a couple of years so I’m excited. We don’t really travel as much. It’s that time of year, Christmas and I’d like to see my family,” said Gabriel Rosales, an air traveler.
The apparent repeat of Thanksgiving movement comes as California reported nearly 33,000 coronavirus cases Tuesday, bringing the state total to well over 1.9 million.
Conditions at El Centro Regional Medical Center in the southeast corner of the state are desperate, even worse than during a summer surge that caught the attention of the governor, hospital officials said.
“We don’t have space for anybody. We’ve been holding patients for days because we can’t get them transferred, can’t get beds for them,” said Lenz, an emergency room physician at the medical center in Imperial County, home to 180,000 people.
Of the 175 patients at the hospital on Monday, 131 had COVID-19. The facility licensed for 161 beds has erected a 50-bed tent in its parking lot and was converting three operating rooms to virus care.
Newsom said a state projection model shows previously unfathomable hospitalization numbers and he’s likely to extend his stay-at-home order for much of the state next week.
Newsom gave Monday’s briefing from his home as he began a 10-day quarantine Sunday for the second time in two months after a staff member tested positive for the virus. The governor was tested and his result came back negative.
Newsom said federal relief aid and more vaccines are both on the way. The first 110,000 doses of the newly approved Moderna vaccine arrived in the state a week after California hospitals administered the first 70,258 doses of the Pfizer vaccine.
The explosion of cases in the last six weeks has California’s death toll climbing. There have been more than 22,000 confirmed deaths since the start of the pandemic and has overwhelmed some hospitals.
California hospitals typically turn to staffing agencies during flu season, when they rely on travel nurses to meet patient care needs. It is the only state in the nation with strict nurse-to-patient ratios requiring hospitals to provide one nurse for every two patients in intensive care and one nurse for every four patients in emergency rooms, for example.
However, those ratio requirements are being waived at many hospitals as virus cases continue to climb.
But the pool of available travel nurses is drying up as demand for them jumped to 44% over the last month, with California, Texas, Florida, New York and Minnesota requesting the most extra staff, according to San Diego-based health care staffing firm Aya Healthcare. It is one of two companies contracted by California to fulfill hospitals’ staffing requests.
“We are hiring like crazy and working insane hours,” said Sophia Morris, vice president of account management at Aya Healthcare.
Ghaly said the state is “lucky to get two-thirds” of its requests for travel nurses fulfilled right now.
It’s a sharp contrast from the spring when Newsom ordered the nation’s first stay-at-home order. As infection rates slowed and hospitals voluntarily suspended elective surgeries for weeks, health care providers from California flew to New York to help their overworked colleagues.
This time, many hospitals are postponing procedures that are not emergencies, said Jan Emerson-Shea, a spokeswoman for the California Hospital Association. California also has opened alternative care facilities for people with less serious illnesses to save hospital beds for the sickest patients.
The Associated Press contributed to this report. Reporting by AP’s Don Thompson. John Antczak and Christopher Weber in Los Angeles, Elliot Spagat in San Diego and Kathleen Ronayne in Sacramento contributed.











