Hospital staffs stretched thin as virus overtakes California hospitals
LOS ANGELES (NewsNation Now) — Medical staffing is stretched increasingly thin as California hospitals scramble to find beds for patients amid a spike of coronavirus cases that threatens to overwhelm the state’s emergency care system.
All of Southern California and the 12-county San Joaquin Valley to the north have exhausted their regular ICU capacity, and some hospitals have begun using “surge” space. Overall, the state’s ICU capacity was just 2.1% on Sunday. Lines formed outside of testing centers, including Los Angeles’ Dodger Stadium, throughout the weekend.
The country’s most populous state has reported more than 1.89 million confirmed coronavirus cases and over 22,000 deaths, according to data complied by Johns Hopkins University.
More than 17,700 people were hospitalized with coronavirus on Sunday, according to the COVID Tracking Project. This is more than double the previous peak reached in July — and a state model that uses current data to forecast future trends shows the number could reach 75,000 by mid-January.
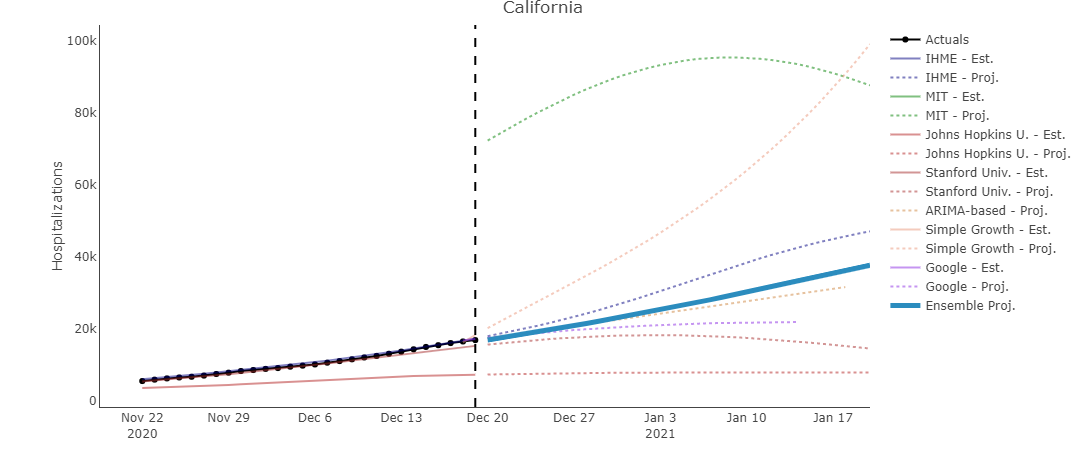
The black box (left) represents the current number of hospitalized COVID patients in California. The blue box represents the forecasted number of hospitalized patients at the 30 day mark based on models for California.
In hard-hit Los Angeles County, Nerissa Black, a nurse at Henry Mayo Newhall Hospital, estimated she’s been averaging less than 10 minutes of care per patient every hour. That includes not just bedside care, but donning gear, writing up charts, reviewing lab results and conferring with doctors, she said.
“And the patients who are coming in are more sick now than they’ve ever been, because a lot of people are waiting before they get care. So when they do come in, they’re really, really sick,” Black said Sunday.
The enormous crush of cases in the last six weeks has California’s death toll spiraling ever higher.
Across Los Angeles County at UCLA Health Santa Monica Medical Center, nurse Wendy Macedo said all 25 beds on her unit are filled with COVID-19 patients. She said a ward on another floor that had been devoted to orthopedic patients has been converted to care for people who have tested positive for the virus. Nurses are working longer shifts, and more of them, she said. There are nearly 5,550 people hospitalized with COVID-19 in Los Angeles County alone.
“The more patients we have, the more there’s a risk of making a mistake, especially if we’re rushing,” Macedo said Sunday. ”Obviously we’re trying to avoid that, but we’re only human.”
California was experiencing “some of the darkest days of our COVID-19 surge,” Gov. Gavin Newsom said, but there was some light Sunday as a working group of scientists and experts endorsed a vaccine developed by Moderna. The step clears the way for the drug to be distributed throughout California and other Western states that reviewed it separately from the U.S. Food and Drug Administration.
Shipments of the vaccine are expected to arrive in California early this week, but it could be months before it’s available for the general public, officials said.
“Until vaccines are available more widely across the state, it’s critical that all Californians do their part to stop the surge by staying at home and wearing a mask when leaving home for essential work and needs,” Newsom said.
Newsom is currently quarantining for 10 days after one of his staffers tested positive for COVID-19, according to a spokesperson for the governor’s office. The staffer tested positive Sunday afternoon, the spokesperson stated. Newsom was then tested and his result came back negative.
Until vaccinations become widespread, hospitals were preparing for the possibility of rationing care. Many hospitals already have implemented emergency procedures to stretch staff and space.
Corona Regional Medical Center southeast of Los Angeles has converted an old emergency room to help handle nearly double the usual number of ICU patients. It’s using space in two disaster tents to triage ER patients because the emergency room is filled with patients who need to be hospitalized.
In hard-hit Fresno County in central California, a new 50-bed alternate care site opened in recent days near the community Regional Medical Center. The beds for COVID-19-negative patients will free up space in area hospitals, where just 13 of some 150 ICU beds were available Friday, said Dan Lynch, the county’s emergency medical services director.
Lynch said he expects they will have to use the Fresno Convention Center, which can accommodate up to 250 patients, given current demand.
Fresno and three neighboring counties also have taken the unprecedented step of sending paramedics on emergency calls to evaluate people. They won’t be taken to the emergency room if they could go to an urgent care facility or wait a few days to talk to their doctors, Lynch said.
Some hospitals have canceled non-essential elective surgeries, such as hip replacements, that might require beds that may soon be needed for COVID-19 patients. Others are increasing staff hours or moving patients to free up space.
Los Angeles County health officials announced Saturday they had modified their health orders to comply with recent U.S. Supreme Court rulings calling for places of worship to be allowed to have outdoor and indoor services, with appropriate health safety precautions.
On Saturday night, Apple Inc. announced that it is temporarily closing all 53 of its stores in California because of the coronavirus outbreak. Under the stay-at-home order in effect for nearly the entire state, retail stores are limited to 20% capacity.















